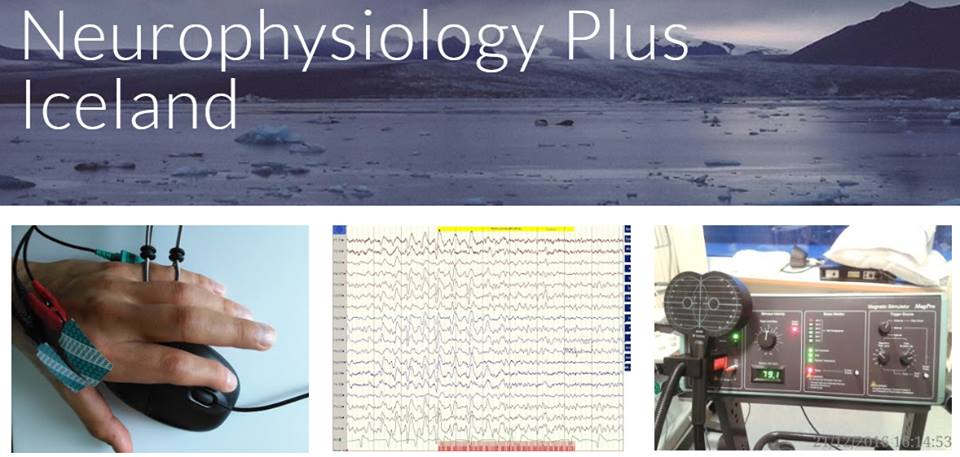
Peripheral nerve injury recovery is assessed in small mammals with nerve conduction studies
Possible research work with an Icelandic company which promotes technologies of regenerative biological tissues, the use of fish skin and fatty acids in the cellular-therapy
21.04.2021, Reykjavik
Motor neurography of the sciatic nerve to right gastrocnemian muscle was used successfuly in a laboratory mouse (Mus musculus) and a laboratory white rat (Rattus norvegicus) on 21st of April 2021. The technique was performed by Ovidiu C. Banea (neurophysiologist) and the Aron Jónasson (biologist) at invitation of Svava Kristinsdóttir, a research scientist from Kerecis and Dr Ingvar H. Ólafsson, neurosurgeon who collaborate with the company.
The nerve microsurgery (microscope) and preparations were performed by Dr Kristín Lilja Eyglóardóttir (Neurosurgeon) and Dr Baldur Tumi Baldursson (Dermatologist).
The "in vivo" motor neurography (nerve conduction study) in an anesthetized laboratory small mammal, might be a summation as a quantitative recovery measurement in a broader Icelandic research project.